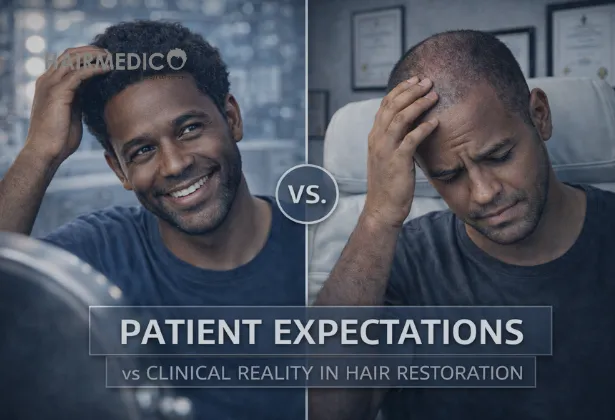
Hair restoration is one of the most emotionally charged fields in modern medicine.
Unlike orthopedic surgery or cardiology, its success is measured not only in millimeters and survival rates, but in identity, self-perception, confidence, and social presence.
Patients do not arrive asking for “follicular unit redistribution.”
They arrive asking for themselves back.
They carry photographs from ten years ago.
They imagine a single procedure restoring a decade of loss.
They expect fullness where biology now offers scarcity.
They hope for reversal rather than reconstruction.
And this is where expectation collides with clinical reality.
As a surgeon, I have learned that the greatest challenge in hair restoration is not technical.
It is conceptual.
The scalp is not a blank canvas.
The donor area is not infinite.
Hair loss is progressive.
And every graft is a non-renewable biological resource.
Modern hair restoration is not about “getting your hair back.”
It is about designing a sustainable future with the biology you still possess.
This article exists to bridge that gap — between what patients hope for and what medicine can ethically deliver.
Hair loss rarely begins in a mirror.
It begins in identity.
Patients describe:
“I no longer recognize myself.”
“People think I am older than I am.”
“I avoid photos.”
“I stopped dating.”
“I lost authority at work.”
By the time a patient contacts a clinic, the request is rarely cosmetic.
It is existential.
This emotional charge fuels unrealistic expectations:
Complete restoration of teenage density
One-session lifetime solution
Zero visibility of surgery
Immediate growth
Permanent immunity to future loss
These expectations are human.
They are also biologically impossible.
Hair restoration is governed by three immutable laws:
The donor area is finite
Hair loss is progressive
Biology cannot be negotiated
A surgeon’s role is not to promise miracles.
It is to protect the patient from future regret.
The most common expectation I encounter is simple:
“I want my entire scalp covered like before.”
What patients do not realize is that:
The average scalp contains 90,000–120,000 hairs
Only 6,000–8,000 follicular units are safely transplantable in a lifetime
Every graft moved is one graft lost forever from the donor zone
This is not a limitation of technique.
It is a limitation of anatomy.
Hair transplantation is a redistribution procedure, not a regeneration therapy.
You are moving resources from a permanent zone to a balding zone.
You are not creating new hair.
Therefore, full density everywhere is mathematically impossible.
The art of hair restoration is strategic illusion:
Prioritize the frontal third
Create optical density
Respect future loss
Preserve donor capital
A patient who demands “everything, everywhere, now”
is a patient at risk of irreversible harm.
The modern patient is educated — but misinformed.
They arrive with:
TikTok transformations
YouTube “day 7 miracles”
Instagram hairlines
Marketing promises
What is rarely shown:
Donor depletion
Patchy overharvesting
Shock loss
Fibrotic recipient beds
Progressive thinning behind transplanted zones
The five-year reality
A photo is a moment.
A transplant is a lifetime.
This is why ethical clinics emphasize long-term planning, as seen in medically documented outcomes such as those presented in Hairmedico’s Before & After cases, where progression, density management, and donor integrity are visible across time.
A surgeon who sells fantasy sells future damage.
Patients speak in visual terms:
“I want it thick.”
“I want it full.”
“I want no scalp visible.”
Surgeons speak in:
Follicular unit density
Vascular supply
Incision trauma
Ischemic risk
There is a biological ceiling to density per square centimeter.
Exceed it, and you compromise:
Blood flow
Graft survival
Healing
Texture
Long-term appearance
High density in one session increases:
Necrosis risk
Poor growth
Cobblestoning
Chronic inflammation
True density is built over time, not forced in one act.
The clinical reality is that natural results require restraint.
Marketing often promotes:
“One day. One surgery. Lifetime result.”
This narrative is dangerous.
Hair loss does not stop because you had surgery.
Transplanted hair is permanent.
Native hair is not.
Without medical management:
The surrounding hair continues to miniaturize
Gaps appear
The transplant becomes isolated
The design ages poorly
Responsible hair restoration is a longitudinal treatment, not a single event.
This is why comprehensive care models include:
Long-term planning
Medical therapy
Follow-up strategy
Donor preservation
Staged procedures when necessary
Patients who understand this achieve harmony.
Patients who reject it experience disappointment.
Not more grafts.
Not cheaper prices.
Not faster procedures.
They need:
Truth
Strategy
Biological respect
Ethical restraint
Long-term vision
This is why education is as important as surgery.
It is also why transparent clinical dialogue, such as the frameworks explained in Hairmedico’s Questions & Answers, protects patients from irreversible mistakes.
A surgeon’s duty is not to fulfill desire.
It is to design sustainability.
| Patient Expectation | Clinical Reality | Medical Rationale |
|---|---|---|
| Full scalp density everywhere | Strategic density in priority zones | Donor supply is finite |
| One surgery for life | Long-term staged planning | Hair loss is progressive |
| Immediate visible growth | Delayed biological growth | Follicles require cycling |
| Unlimited graft availability | Limited donor capacity | Overharvesting causes permanent damage |
| Social-media hairlines | Age-appropriate hairline design | Facial aging must be respected |
| Dense packing in one session | Controlled density over time | Vascular survival limits |
| No future hair loss | Ongoing medical management | Native hair continues to miniaturize |
Many failures in hair restoration do not appear in the first year.
They emerge slowly.
Poor planning results in:
Isolated frontal islands
Visible donor thinning
Artificial hairline aging
Lack of graft reserve for correction
Successful cases, by contrast, show:
Donor stability
Harmonious aging
Consistent density transitions
Preserved revision capacity
Time is the ultimate judge of surgical ethics.
Ethical surgeons must sometimes refuse surgery.
They must sometimes recommend delay.
They must sometimes say “this is not achievable.”
This is not pessimism.
It is professionalism.
Medicine is not about satisfying desire.
It is about preventing harm.
Hair restoration is not a cosmetic shortcut.
It is a lifelong biological strategy.
Expectation management is not an accessory to surgery.
It is the surgery before the surgery.
When expectations align with biology, results endure.
When they do not, regret follows.
The role of the surgeon is not to sell hope.
It is to protect the future.
Your consultant is ready to answer your hair transplant questions, and you can also get a personalized online hair analysis.