“Hair transplant without shaving” is one of the most searched phrases among professionals, executives, public figures, and patients who cannot afford visible downtime. The promise is compelling: restore hair while keeping your existing hairstyle intact.
However, this topic is also one of the most misunderstood and over-marketed procedures in hair restoration.
Not everyone is a candidate.
Not every hair loss pattern allows it.
And when done incorrectly, unshaven procedures can compromise both results and donor safety.
This article is a professional, medical-grade analysis, written in the clinical philosophy of Dr. Arslan Musbeh, to answer one essential question:
Who is really a good candidate for a hair transplant without shaving—and who is not?
A true unshaven hair transplant means:
The recipient area is not shaved
The surrounding hair remains intact
Grafts are implanted between existing hairs
Donor hair may be partially or selectively trimmed, not fully shaved
This is not a single technique—it is an advanced execution strategy that can be applied to FUE or DHI, depending on the case.
Key medical reality:
“No-shave” refers to visual discretion, not to a different biological procedure.
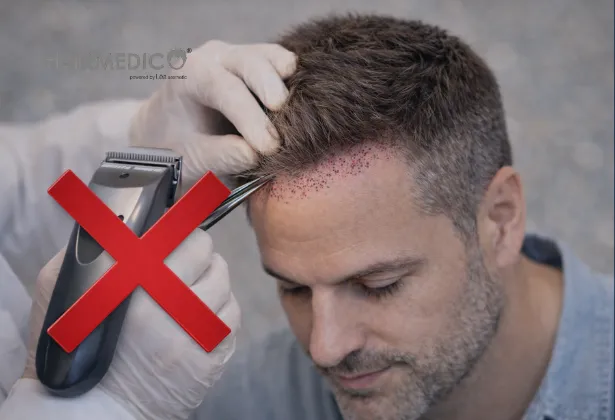
Unshaven procedures significantly increase:
Technical difficulty
Operative time
Risk of graft trauma
Risk of uneven density
For this reason, ethical surgeons do not offer it universally.
At Hairmedico, unshaven transplantation is considered a privilege of anatomy, not a marketing option.
The best candidates have:
Small to medium recession zones
Localized thinning (temples, hairline refinement, crown touch-up)
Norwood scale: I–III (selected cases)
Large bald areas are not suitable.
Unshaven transplantation relies on existing hair to camouflage healing.
Ideal candidates:
Have good native density around the target area
Do not have diffuse thinning
Have stable hair shafts that can hide graft placement
Low-density patients are poor candidates.
Hair caliber matters.
| Hair Type | Suitability |
|---|---|
| Thick hair | Excellent |
| Medium hair | Good |
| Fine hair | Limited |
| Miniaturized hair | Poor |
Thin hair does not provide adequate visual coverage during healing.
Candidates must have:
Controlled or stabilized hair loss
No aggressive ongoing shedding
Realistic long-term expectations
Unshaven procedures are not suitable for rapidly progressing alopecia.
This is critical.
Unshaven hair transplants:
Prioritize natural integration, not maximum density
Often involve fewer grafts per session
Are sometimes part of a staged plan
Patients demanding “maximum density in one session” are not candidates.
Large bald areas require:
Wide access
Full visibility
Dense graft packing
Unshaven techniques limit surgeon visibility and precision in such cases.
Diffuse thinning patients risk:
Shock loss of existing hair
Visual worsening
Poor blending
Shaving is often safer and more controlled.
Unshaven procedures do not compensate for donor limitations.
If the donor area is:
Sparse
Previously overharvested
Structurally compromised
Then discretion should never override safety.
No procedure is truly downtime-free.
Unshaven does not mean:
No redness
No crusting
No healing phase
Patients expecting invisibility rather than discretion are not suitable.
| Criteria | Shaven Transplant | Unshaven Transplant |
|---|---|---|
| Surgical visibility | Maximum | Limited |
| Maximum graft count | High | Moderate |
| Healing camouflage | Low | High |
| Technical difficulty | Standard | Advanced |
| Candidate pool | Broad | Selective |
| Risk if poorly done | Moderate | High |
Unshaven hair transplantation is not superior—it is situational.
A well-indicated shaven transplant will always outperform a poorly indicated unshaven one.
Medical principle:
Technique should follow anatomy, not lifestyle preference.
Both can be used—but only in expert hands.
Better control between existing hairs
Reduced recipient trauma
Preferred for dense native hair zones
Possible but technically demanding
Requires precise channel control
Higher risk if rushed
The choice depends on hair angle, density, and surgical plan—not marketing.
Contrary to popular belief:
Donor area is often partially shaved
Selective trimming is used for extraction
Full invisibility is rare in early days
Ethical surgeons never compromise donor safety for visual discretion.
Mild redness between existing hairs
Small crusts hidden by surrounding hair
Donor area selectively camouflaged
Crusts shed naturally
Redness fades
Visual normality returns
Progressive hair growth
Natural integration
Final density assessment at 12 months
| Myth | Medical Reality |
|---|---|
| No shaving at all | Partial shaving is often necessary |
| No downtime | Healing still occurs |
| Anyone can do it | Only selected candidates |
| Same density as shaved | Usually lower per session |
| Easier procedure | Technically harder |
At Hairmedico, unshaven transplantation follows strict principles:
One patient per day
Surgeon-led planning and execution
Conservative graft strategy
Long-term donor protection
No compromise between discretion and medical ethics
Unshaven is offered only when anatomy allows it—never as a sales tool.
Before choosing an unshaven transplant:
Am I choosing discretion—or avoiding proper surgery?
Is my hair loss pattern suitable long-term?
Who will perform the critical steps?
Can I see healed unshaven cases after 12 months?
If these questions are avoided, caution is advised.
A hair transplant without shaving can be an excellent option—but only for the right patient, with the right anatomy, performed by a surgeon-led team.
When misused, it risks:
Suboptimal density
Poor blending
Donor compromise
In hair restoration, visibility should never dictate biology.
The best results come from correct indication—not convenience.
Your consultant is ready to answer your hair transplant questions, and you can also get a personalized online hair analysis.