Hair loss treatment has evolved from anecdotal remedies to evidence-driven medical protocols. Yet despite decades of research, confusion remains among patients—and even some practitioners—regarding what truly works, how treatments differ mechanistically, and how to plan long-term therapy responsibly. As a hair transplant surgeon and clinician, I approach this topic not from marketing narratives, but from biological evidence, clinical outcomes, and longitudinal patient follow-up.
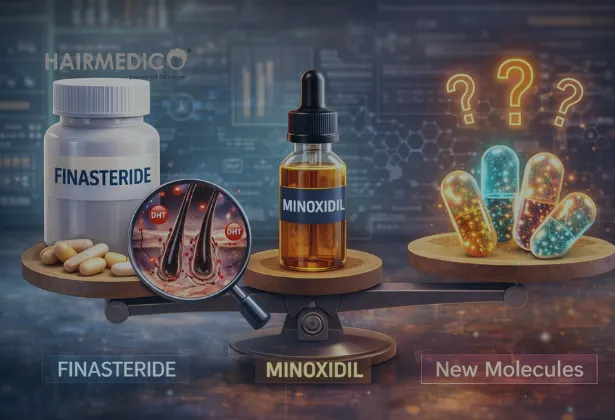
This article provides a rigorous, evidence-based comparison of finasteride, minoxidil, and new-generation molecules emerging in modern hair loss therapy. The objective is clarity: what these treatments do, what they do not do, and how they should—or should not—be combined within a sustainable hair preservation strategy.
Hair loss is not a cosmetic inconvenience. It is a progressive biological process. Any effective intervention must be evaluated not by short-term regrowth, but by its capacity to slow follicular aging, preserve existing hair, and integrate ethically with surgical planning when needed.
Androgenetic alopecia is not caused by a single factor. It is the clinical result of genetically programmed follicular sensitivity to androgens, chronic micro-inflammation, altered follicular cycling, and progressive miniaturization. Hair follicles do not “die” suddenly. They gradually lose diameter, anagen duration shortens, and regenerative signaling declines.
Key biological features include:
• Dihydrotestosterone-mediated follicular sensitivity
• Progressive shortening of the anagen phase
• Increased perifollicular inflammation
• Dermal papilla signaling impairment
• Eventual follicular miniaturization
Any treatment must therefore be judged by how it interacts with these mechanisms—not by isolated cosmetic outcomes.
Finasteride is a type II 5-alpha-reductase inhibitor. Its mechanism is precise: it reduces the conversion of testosterone to dihydrotestosterone (DHT), the androgen most strongly implicated in follicular miniaturization in genetically susceptible individuals.
Finasteride lowers scalp and serum DHT levels by approximately 60–70 percent. By reducing DHT binding at the follicular level, it slows the miniaturization process rather than directly stimulating growth.
Clinical implications:
• Slows progression rather than “regrowing” hair
• Most effective in early to moderate stages
• Acts systemically, not locally
• Requires long-term, consistent use
Large randomized controlled trials have consistently shown that finasteride stabilizes hair loss and preserves density over 5–10 years when started early. Discontinuation leads to reversal of benefits within months, underscoring that it does not cure alopecia but controls its biological driver.
Finasteride remains one of the most debated molecules due to concerns around sexual and psychological side effects. From a clinical standpoint, these effects are real but statistically uncommon and dose-dependent. Proper patient selection, informed consent, and medical supervision are essential.
Finasteride should never be prescribed casually or dismissed emotionally. It is a medical therapy that demands responsibility.
For patients seeking a medically supervised, conservative approach to hair preservation, finasteride remains a cornerstone therapy when appropriately indicated, as outlined in long-term protocols used in advanced hair restoration planning such as those described on https://hairmedico.com/greffe-de-cheveux.
Minoxidil operates through a fundamentally different mechanism. Originally an antihypertensive drug, its hair growth effects were discovered incidentally.
Minoxidil is a potassium channel opener that enhances blood flow, prolongs the anagen phase, and increases follicular size temporarily. It does not address the androgenic cause of hair loss.
Clinical effects:
• Extends growth phase
• Increases hair shaft diameter
• Improves local vascular support
• Does not block DHT
Minoxidil is effective in increasing visible density and slowing shedding, particularly in early stages. However, its effects are cosmetic and functional rather than disease-modifying. When discontinued, treated hairs are lost.
Minoxidil does not prevent long-term follicular aging. In isolation, it may mask progression rather than halt it. This distinction is critical for patient counseling.
Minoxidil is best understood as a supportive agent, not a standalone solution.
| Parameter | Finasteride | Minoxidil |
|---|---|---|
| Primary action | DHT suppression | Growth stimulation |
| Addresses root cause | Yes | No |
| Hormonal involvement | Systemic | None |
| Onset of effect | 3–6 months | 2–4 months |
| Long-term stabilization | Strong | Limited |
| Discontinuation effect | Rapid loss of benefit | Rapid loss of benefit |
| Role in surgery planning | Critical | Supportive |
The misconception that one can replace the other is biologically inaccurate. They serve different roles and, when indicated, are often complementary.
The last decade has seen the emergence of new therapeutic targets aimed at improving efficacy while minimizing systemic risk.
Topical formulations aim to reduce systemic exposure while maintaining local DHT suppression. Early data suggests partial efficacy, though absorption variability remains a concern.
Peptide complexes and autologous growth factor therapies aim to improve follicular micro-environment rather than hormonal pathways. These include PRP-based strategies, discussed as adjunctive—not primary—therapies in surgical planning such as those integrated into protocols on https://hairmedico.com/techniques/greffe-de-cheveux-fue.
Experimental molecules targeting follicular stem cell signaling represent a promising frontier. However, most remain in early-phase trials and are not yet clinically validated.
Emerging evidence highlights the role of chronic micro-inflammation and scalp microbiome imbalance in follicular aging. Novel molecules targeting inflammatory cascades may complement existing treatments rather than replace them.
Despite innovation, no new molecule has yet replaced finasteride as the most effective DHT-modulating agent with long-term data. Many “next-generation” treatments improve tolerance, convenience, or adjunctive benefit, but none reverse follicular aging.
Scientific reality:
• Follicular aging is not reversible
• Stem cell exhaustion cannot be reset
• Treatments slow progression, not biology
Any claim suggesting “hair loss reversal” should be met with clinical skepticism.
An effective protocol is not about stacking products. It is about biological logic.
Evidence-based strategy:
• Finasteride to control androgenic drive
• Minoxidil to support growth kinetics
• Adjunctive therapies to optimize scalp environment
• Surgical intervention only when stability is achieved
This integrated approach aligns with ethical hair restoration principles emphasized in long-term planning models such as those outlined at https://hairmedico.com/avant-et-apres.
Hair transplantation redistributes follicles. It does not stop the disease. Ignoring medical therapy leads to progressive native hair loss around transplanted areas, resulting in unnatural patterns over time.
From a surgical standpoint:
• Finasteride preserves surrounding native hair
• Minoxidil improves post-operative growth kinetics
• Stabilization precedes transplantation
Failure to integrate medical therapy is not conservative—it is negligent.
• “I’ll use minoxidil instead of finasteride” – biologically flawed
• “New molecules are safer and stronger” – unproven
• “I can stop after transplant” – incorrect
• “Side effects are guaranteed” – statistically inaccurate
Education is as important as prescription.
Hair loss treatment should not be driven by fear or marketing. It must be guided by biology, evidence, and long-term responsibility.
Finasteride remains the most effective disease-modifying therapy for androgenetic alopecia. Minoxidil remains a valuable supportive agent. New molecules expand our toolbox but do not rewrite biological limits.
In my clinical philosophy, success is not measured by short-term density gains, but by preservation of identity, proportion, and harmony over decades. Hair restoration is a medical journey—not a product choice.
Your consultant is ready to answer your hair transplant questions, and you can also get a personalized online hair analysis.